Oral Radiology CBCT Case of the Month #1
Greetings to all, and a special nod to mathematics lovers on this Pi Day! Today, we're finally kicking off our long-anticipated series: Oral Radiology CBCT Case of the Week. The inaugural case offers an important lesson that a dental observation might play a pivotal role in a patient's overall health.
A simple, yet profound incident in our radiology practice has made me reflect on the significant impacts of our daily work. Surprisingly, most dental professionals, and even some radiologists often overlook these routine findings. Yet, it's some of these common incidental findings that can ultimately lead to life-changing outcomes for our patients.
Patient Information
Our case study involves a 56-year-old woman who just so happens to be the mother of one of my students. The doctor notes with the referral stated, “Dx #5 for possibly vertical root fx and subsequent immediate implant in the AEGD. Please check TMJ left side slides upon opening.”
Radiographic Images
Take a moment to examine the provided CBCT images:
Did you see it? If not, scroll through it again, and this time focus on the bottom part of the volume. Look to the left (always referring to the patient’s left, so the right side of the screen) of the airway almost at the bottom of the volume.
Did anything catch your eye? If not, take a closer look at the bottom part of the volume, in particular, a small hyperdensity to the left of the airway, approximately at the level of the C4 vertebrae.
Differential Diagnosis
What is the most likely source of this hyperdensity in the left neck?
Thyroid Cartilage Try again. Thyroid Cartilage calcification is seen in the image, but it is just posterior to the lateral border of the airway.
Parotid Gland Try again. This is too far inferior to be the parotid artery.
Submandibular Gland Nice try, but this is incorrect. You can see the submandibular gland if you scroll superior to where this calcification lies. It is both superior and anterior to the calcification.
Carotid Artery Congratulations, you are correct! This calcification lies within the carotid artery, which is medial to the sternocleidomastoid muscle and lateral to the posterior border of the airway.
Discussion: How to identify carotid artery calcifications in a Cone Beam CT
You may recognize the large muscle seen just posterolateral to that calcification as the sternocleidomastoid. That is a good landmark for determining if a calcification lies within an artery or not. Another good landmark is comparing with the airway and the location of the thyroid cartilage. The thyroid cartilage frequently calcifies (as seen in this case) so it can mimic the appearance of a calcified carotid artery atheroma. But the biggest difference is that the thyroid cartilage (and triticeal cartilage) always lies very close to the airway, while the carotid artery lies between the posterolateral border of the airway and the sternocleidomastoid muscle, usually a little further away from the airway.
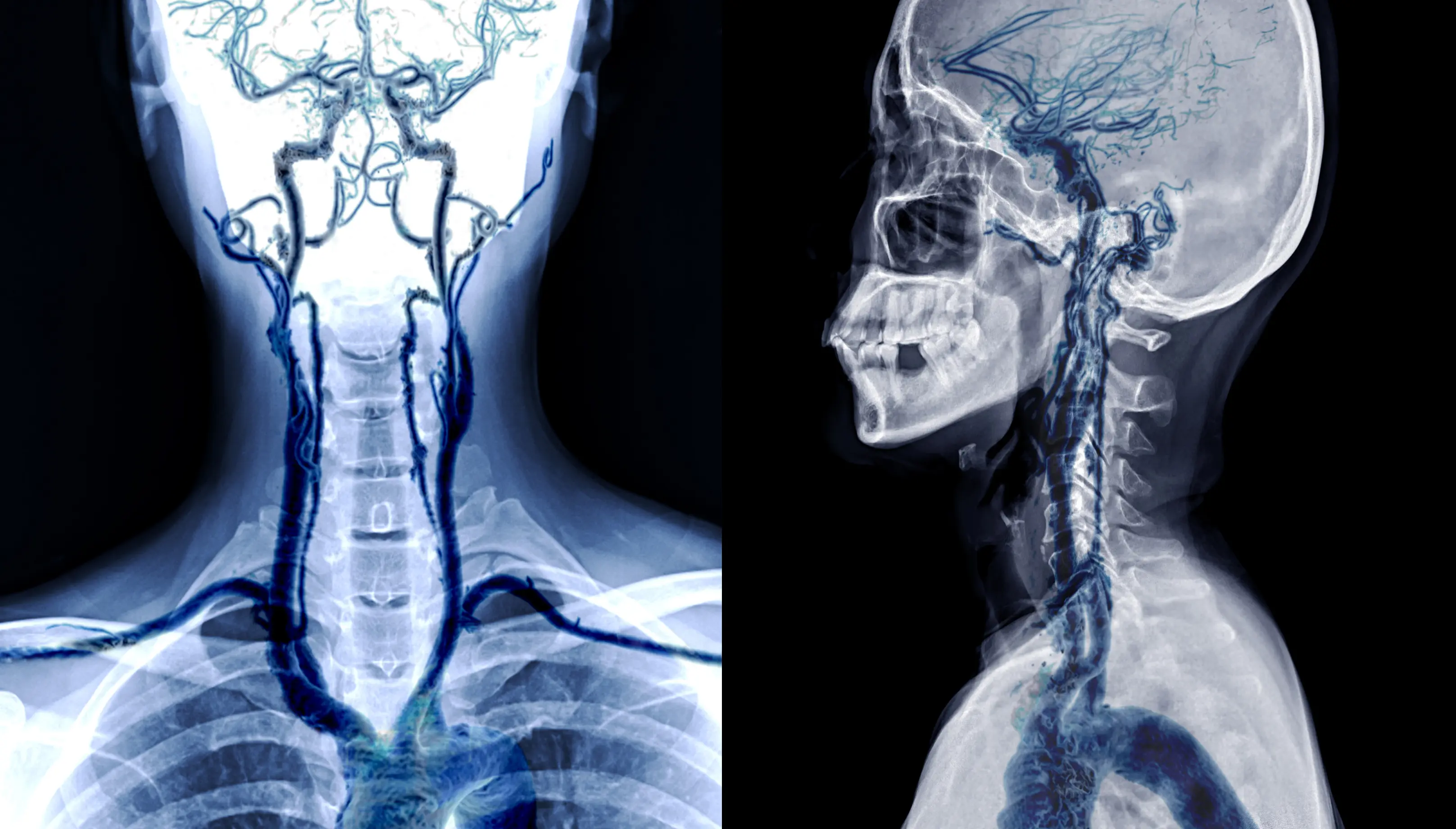 Carotid arteries seen lateral to the airway, with the bifurcation near the
level of C4
Carotid arteries seen lateral to the airway, with the bifurcation near the
level of C4
You can also see the outline of the carotid artery to recognize that the calcification lies within it. Cone beam CTs do not show soft tissue structures like muscles and arteries with great contrast, but they can be seen. This calcification lies right at the expected location – the carotid bifurcation. The common carotid artery bifurcates into the internal and external carotid arteries, usually around the level of C3 or C4. If you scroll superiorly from the calcification in the axial slices in this case, you can just make out the external carotid artery branching anteriorly and the internal carotid artery branching posteriorly.

Axial slice displaying carotid artery calcification.
Conclusion
Although I didn’t think much of it at the time, the student thanked me profusely for noticing this common incidental finding and including a recommendation in the report. She explained in an email,
“You noted the calcifications and she made an appointment with her doctor for a checkup with your notes in mind. I can’t remember exactly what tests they ran off the top of my head but she ended up needing to be flight for lifed to Denver that day. She ended up having a quadruple bypass- 100%, 100%, 90, and 80% blockages. Since then she’s had 6 [stents] placed even being on medication and a significant amount of weight loss. She mentioned to her cardiologist that you found calcifications in her CBCT and he said every single patient he sees has those calcifications and was impressed that you mentioned it to her because it’s very seldom that dentists pass that information along to their patients. She never ended up having an MI [myocardial infarction, aka heart attack] because we caught it ‘in time’. Since then, my team members and I have seen MANY patients with these calcifications and have suggested they go see their PCPs. I think this is very important for an overall holistic approach to health care.”
So, in the opinion of this cardiologist, this finding likely prevented this patient’s mother from suffering a heart attack (Myocardial Infarction). I surmise that the physician may have first performed an ultrasound on the carotid arteries to look for blockage, but to diagnose coronary artery blockage, they must have done a cardiogram. Even in hindsight, it’s incredible that they found that degree of blockage when all we saw was a small calcification in the left neck.
I wonder if this small incidental finding would have been taken as seriously if it didn’t happen to be in one of my student’s mothers. But shouldn’t we treat every patient as if they were our own family? I was glad to read that at least for her and her team members, this experience made them look for, and find this important finding in other patients.
